Dans la lutte contre l’épidémie de Covid-19, n’est-il pas temps, les évidences scientifiques rassurantes à ce propos s’accumulant, de laisser place au plan D, comme démocratique et pluriel, plus respectueux de la santé tant physique que psychique de chacun?
De plus en plus d’études scientifiques statistiques comparatives montrent que les mesures non-pharmacologiques restrictives comme le confinement généralisé et l’arrêt des activités dites non-essentielles prises pour lutter contre l’épidémie de Covid-19 pourraient être non-efficaces, voire en fait contre-productives [1-4]. Cela peut paraître contre-intuitif et pourtant qui affirmerait aujourd’hui que la terre est plate ?
Un modèle scientifique est valable tant que la réalité le valide et non l’inverse. Les modèles théoriques utilisés pour prédire l’évolution de l’épidémies sont multivariés et difficiles à valider de manière univoque et correcte par l’expérience réelle sur le terrain qui est très complexe. Ces modèles seraient en fait trop simplifiés et attribueraient tout le bénéfice aux dernières mesures prisent les plus restrictives sans tenir compte des mesures précédentes, de l’évolution naturelle et dynamique de l’épidémie, du pourcentage de la population naturellement immunisée contre le coronavirus … [1,2].
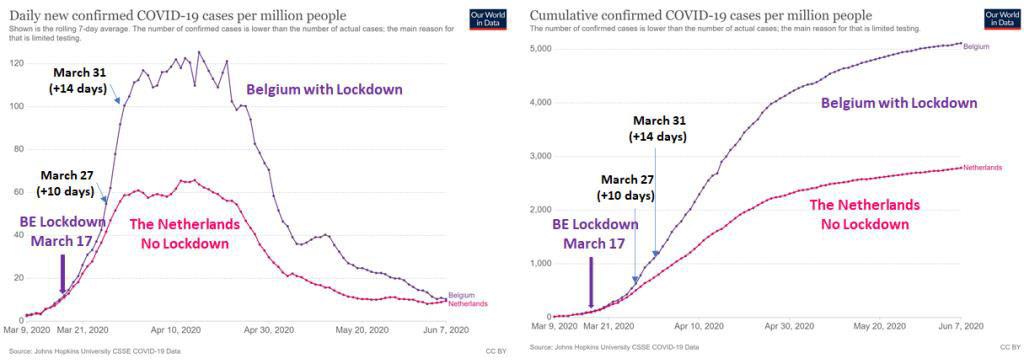
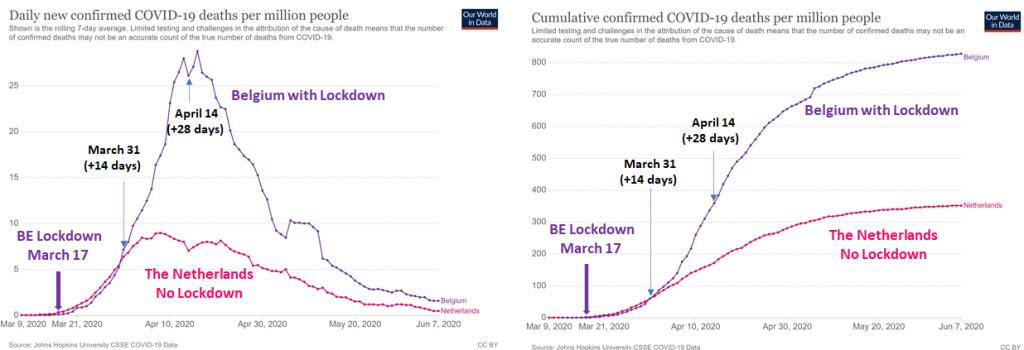
Voici d’ailleurs deux figures qui comparent la situation épidémiologique en termes de cas et de morts liés au Covid (source https://ourworldindata.org/) en Belgique et chez son voisin aux Pays-Bas, lors de la première vague de l’épidémie en 2020 (Fig. 1 et Fig. 2). Cette simple comparaison, sans aller dans le détail, ni les analyses statistiques fines, faites par les épidémiologistes des études [1-4], interpelle en tout cas : Le confinement strict du 17 mars
en Belgique semble suivi 10 jours après d’une accélération franches des contaminations et ensuite de la mortalité dans les semaines qui suivent, par rapport aux Pays-Bas qui n’ont, eux, pas optés pour un confinement strict et privilégié l’immunité naturelle. Les deux pays se trouvaient dans des situations pourtant comparables avant le confinement belge.
Une des explications (il pourrait y avoir d’autres facteurs) : On confine les malades et les personnes saines ensemble et on augmente, ainsi, fortement la transmission dans les foyers. C’est surtout désastreux pour les gens les plus à risques dans les maisons de repos qui sont contaminés par le personnel soignant et une fois que le virus arrive et tout le monde est confiné, c’est la catastrophe… Il faudrait en fait des mesures sélectives et uniquement pour les personnes à risques qui sont très bien identifiées pour le Covid et ont une probabilité de décès 1000 fois plus importantes que les autres, et laisser les autres vivre une vie normale pour que l’épidémie passe au plus vite, dixit Prof. J. P.A. Ioannidis, de l’université américaine de Stanford, l’un des plus célèbre et respecté épidémiologiste au monde [1,2]. En ralentissant la transmission d’hôte à hôte par ces mesures, on rallonge l’épidémie et augmente le risque de mutation et l’émergence de nouveaux mutants qui pourraient échapper à l’immunité de groupe déjà acquise et être plus contagieux [5,6,7,8].
Les mesures non-pharmacologiques généralisées engendrent également des surcoûts économiques, humains et sociétaux énormes, sans bénéfices prouvés par rapport à des mesures ciblées uniquement sur les personnes à risques, et fort supérieur à tous bénéfices escomptés [9,10,11].
De surcroit, si des dire même de l’OMS [12,13], le port du masque médical de type FFP2 (les masques non médicaux aurait-eux eu une efficacité limitée [14,15]) a une utilité pour le personnel soignant directement en contact avec les malades, les malades symptomatiques et aussi sans doute pour les personnes à risques comme protection supplémentaire, le port généralisé pour les personnes ne présentant pas de symptômes apparents de la maladie n’a pas ou peu de justifications scientifiques [12,13,14,15,16,17,18]. L’OMS, après s’être prononcé contre [12] semble l’accepter [13], vu la forte demande des états pour rassurer les populations, comme une mesure plutôt de l’ordre psychologique [13], voire d’un talisman qui rassure [16] et en l’absence de preuves scientifiques concluantes dans ce cas [12,13,15,16,18], et de la faible contagiosité des asymptomatiques [12,13,19,20,21,22,23]. Si le masque s’avère utile pour bloquer les gouttelettes de salives plus larges (typiquement plus large que 5 mm) pour les malades symptomatiques, les fines gouttelettes de type aérosol, qui pourraient être virtuellement aussi petites que le virus lui-même (qui lui est d’une taille entre 60 à 120 nm, soit environ 1000 fois plus petits que les mailles des masques typiquement entre 50 et 500 mm [15]) ne seraient, elles, pas efficacement bloquées [15,17,18]. Cette transmission de type aérosol courte portée semblent de plus en plus être un mode représentatif de la transmission [15,17,18 ,24]. A fortiori, aussi, le port du masque en extérieur où le risque de contamination est très faible [25,26], ou pour les enfants rarement symptomatiques et peu contagieux [27] semblent se faire en dépit de toute balance bénéfice-risque et bon sens. Car si les preuves scientifiques pour l’utilité du masque généralisé à toute la population manquent [12,13,15], les risques de son impact négatif sur la santé physique et mentale ont été démontrés, par exemple [15,28,29,30,31] et Table 1. Le port du masque, le confinement, la pratique de la distanciation sociale et le stress et l’isolation associés peuvent de plus affaiblir notre système immunitaire [8,15,32] et pourraient donc contribuer à augmenter paradoxalement le risque de formes sévères (et donc beaucoup plus contagieuses), d’hospitalisations, de décès et de contagions, surtout dans les populations non à risques où le bénéfice de ces mesures n’est pas démontré [1,2,3,4, 9,12,13,15].
![Table 1 de [15].](https://img.static-rmg.be/a/view/q75/w/h/3700366/02ac4d1e1ea7ca91a4a5b032c591fa01-jpg.jpg)
Nous pourrions continuer sur les tests PCR dont le nombre de cycle d’amplification (Ct ou cycle threshold) au coefficient de plus de 35, choisit initialement, sans doute, comme précaution extrême, signifie une sensibilité telle qu’une personne testée positive, peut l’être sans être malade ou contagieuse [33,34,35,36], ce que l’OMS a récemment confirmé [34], ou sur la létalité de la maladie qui a été revue fortement à la baisse [9,15,37,38] …
Alors, la réalité est complexe, et malgré toute son intelligence, le savoir humain reste limité. Le risque zéro n’existant pas, à l’ère du tout digital, ne serait-il pas bon de se rappeler que la vie n’est pas binaire, mais avant tout complexe, libre et imprévisible ? Ceci est d’ailleurs formalisé par le deuxième grand principe de la thermodynamique qui nous explique que toute action sur un système entraîne une contre-réaction pour contrer celle-ci. Alors n’est-il pas temps de sortir du plan A, absolu et unique pour tous, de sa logique binaire (faire ou ne pas faire), restrictive et infantilisante, ou une loi dictée d’en haut s’applique pour tous, malgré les situations et rationnels si différents de chaque cas individuel et pourrait bien faire penser au « plan » d’un régime marxiste qui n’a pas fonctionné ? N’est-il pas temps, les évidences scientifiques rassurantes à ce propos s’accumulant, de laisser place au plan D’, comme démocratique et pluriel, plus respectueux de la santé tant physique que psychique de chacun, et donc tenant compte de risque de la déprime (D’) ? Celui de la libre entreprise, de la liberté de chaque généraliste de soigner et prescrire [39,40], celui qui laisse chaque citoyen libre et responsable de gérer l’entropie de la vie en minimisant son risque et maximisant son bénéfice pour maximiser le gain collectif ? N’est-ce pas d’ailleurs, le modèle que plusieurs millénaires de sagesse et d’intelligence humaine ont reconnu comme le seul qui ait fait ses preuves, et si pas le meilleur, en tous cas le moins pire ?
Aryan Afzalian, Ingénieur et Docteur en Sciences Appliquées
Références:
[1] Assessing mandatory stay?at?home and business closure effects on the spread of Covid-19: https://onlinelibrary.wiley.com/doi/epdf/10.1111/eci.13484
[3] Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation: https://doi.org/10.3389/fpubh.2020.604339
[4] Lansiaux et al (2021): Assessing the efficiency of COVID-19 NPIs in France: a retrospective study using a novel methodology. Preprint. https://doi.org/10.6084/m9.figshare.14195228.v1
[5] Transmission bottlenecks as determinants of virulence in rapidly evolving pathogens | PNAS
[6] SARS-CoV-2 spike D614G change enhances replication and transmission | Nature
[7] Mechanisms and Concepts in RNA Virus Population Dynamics and Evolution | Annual Review of Virology (annualreviews.org)
[8] Notes et présentation de l’intervention du Dr Vanden Bossche au Sommet sur la vaccination qui a eu lieu dans l’Ohio entre le 1 et le 3 mars 2021, organisé par le Biogate Scientific Center Pvt Ltd.
[9] COVID-19: Rethinking the Lockdown Groupthink: https://doi.org/10.3389/fpubh.2021.625778. Les dommages collatéraux massifs des mesures sont au moins 10 fois plus élevés que tout bénéfice qu’on pourrait espérer. Il s’agit du Mea Culpa honnête et documenté d’un expert du gouvernement Canadien illustré par près de 300 références. Errare humanum est, perseverare diabolicum…
[10] Les mesures de lutte contre le Covid-19 ont aussi des coûts! Elles pèsent de façon disproportionnée sur les pauvres et les vulnérables, https://covidrationnel.be/2021/03/03/les-mesures-de-lutte-contre-le-covid-19-ont-aussi-des-couts-elles-pesent-de-facon-disproportionnee-sur-les-pauvres-et-les-vulnerables/
[11] https://inequality.org/great-divide/updates-billionaire-pandemic/
[12] World Health Organization. Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak. Geneva, Switzerland; 2020. https://apps.who.int/iris/handle/10665/330987
[13] World Health Organization. Advice on the use of masks in the context of COVID-19. Interim guidance 5 June 2020. https://apps.who.int/iris/handle/10665/332293 : Many countries have recommended the use of fabric masks/face coverings for the general public. At the present time, the widespread use of masks by healthy people in the community setting is not yet supported by high quality or direct scientific evidence and there are potential benefits and harms to consider (see below).
[14] MacIntyre C.R., Seale H., Dung T.C., Hien N.T., Nga P.T., Chughtai A.A. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ open. 2015;5. This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection.
[15] Vainshelboim B. Facemasks in the COVID-19 era: A health hypothesis. Med Hypotheses. 2021;146:110411. doi:10.1016/j.mehy.2020.110411 : Review sur les masques, leur utilité et leur effets sur la santé. Many countries across the globe utilized medical and non-medical facemasks as non-pharmaceutical intervention for reducing the transmission and infectivity of coronavirus disease-2019 (COVID-19). Although, scientific evidence supporting facemasks’ efficacy is lacking, adverse physiological, psychological and health effects are established. Is has been hypothesized that facemasks have compromised safety and efficacy profile and should be avoided from use. The current article comprehensively summarizes scientific evidences with respect to wearing facemasks in the COVID-19 era, providing prosper information for public health and decisions making.
[16] Universal Masking in Hospitals in the Covid-19 Era, N Engl J Med 2020; 382:e63 DOI: 10.1056/NEJMp2006372. Article sur l’usage généralisés du masque en milieux hospitalier. We know that wearing a mask outside health care facilities offers little, if any, protection from infection. Public health authorities define a significant exposure to Covid-19 as face-to-face contact within 6 feet with a patient with symptomatic Covid-19 that is sustained for at least a few minutes (and some say more than 10 minutes or even 30 minutes). The chance of catching Covid-19 from a passing interaction in a public space is therefore minimal. In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic. There may be additional benefits to broad masking policies that extend beyond their technical contribution to reducing pathogen transmission. Masks are visible reminders of an otherwise invisible yet widely prevalent pathogen and may remind people of the importance of social distancing and other infection-control measures.
[17] https://www.cidrap.umn.edu/news-perspective/2020/04/commentary-masks-all-covid-19-not-based-sound-data. : Pas vraiment d’évidence pour le masque pour tous, surtout que risque de transmission par aérosol.
[18] Respiratory virus shedding in exhaled breath and efficacy of face masks https://www.nature.com/articles/s41591-020-0843-2: Intérêt du masque pour gouttelette chez symptomatiques, chez asymptomatiques faibles différences surtout pour transmission aérosol qui est observée pour les coronavirus.
[19] A study on infectivity of asymptomatic SARS-CoV-2 carriers, Respir Med. 2020 Aug; 169: 106026. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7219423/: 455 contacts who were exposed to the asymptomatic COVID-19 virus carrier became the subjects of our research. The median contact time for patients was four days and that for family members was five days. All CT images showed no sign of COVID-19 infection. No severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections was detected in 455 contacts by nucleic acid test. In summary, all the 455 contacts were excluded from SARS-CoV-2 infection and we conclude that the infectivity of some asymptomatic SARS-CoV-2 carriers might be weak.
[20] Contact Settings and Risk for Transmission in 3410 Close Contacts of Patients With COVID-19 in Guangzhou, China. https://www.acpjournals.org/doi/10.7326/M20-2671: Infection max dans foyer (10x plus que à l’hôpital et 100x plus que dans transport en commun) et augmente fortement avec la force des symptomes (asymptomatiques 10 à 20 fois moins contagieux) et la toux.: Among 3410 close contacts, 127 (3.7% [95% CI, 3.1% to 4.4%]) were secondarily infected. Of these 127 persons, 8 (6.3% [CI, 2.1% to 10.5%]) were asymptomatic. Of the 119 symptomatic cases, 20 (16.8%) were defined as mild, 87 (73.1%) as moderate, and 12 (10.1%) as severe or critical. Compared with the household setting (10.3%), the secondary attack rate was lower
for exposures in health care settings (1.0%; odds ratio [OR], 0.09 [CI, 0.04 to 0.20]) and on public transportation (0.1%; OR, 0.01 [CI, 0.00 to 0.08]). The secondary attack rate increased with the severity of index cases, from 0.3% (CI, 0.0% to 1.0%) for asymptomatic to 3.3% (CI, 1.8% to 4.8%) for mild, 5.6% (CI, 4.4% to 6.8%) for moderate, and 6.2% (CI, 3.2% to 9.1%) for severe or critical cases. Index cases with expectoration were associated with higher risk for secondary infection (13.6% vs. 3.0% for index cases without expectoration; OR, 4.81 [CI, 3.35 to 6.93]).
[21] Analysis of Asymptomatic and Presymptomatic Transmission in SARS-CoV-2 Outbreak, Germany, 2020, EID Journal, 27 (4), April 2021, https://wwwnc.cdc.gov/eid/article/27/4/20-4576_article: We determined secondary attack rates (SAR) among close contacts of 59 asymptomatic and symptomatic coronavirus disease case-patients by presymptomatic and symptomatic exposure. We observed no transmission from asymptomatic case-patients and highest SAR through presymptomatic exposure. Rapid quarantine of close contacts with or without symptoms is needed to prevent presymptomatic transmission.
[22] Coronavirus Disease Outbreak in Call Center, South Korea, EID Journal,Volume 26, Number 8–August 2020: https://wwwnc.cdc.gov/eid/article/26/8/20-1274_article#r6: We describe the epidemiology of a coronavirus disease (COVID-19) outbreak in a call center in South Korea. We obtained information on demographic characteristics by using standardized epidemiologic investigation forms. We performed descriptive analyses and reported the results as frequencies and proportions for categoric variables. Of 1,143 persons who were tested for COVID-19, a total of 97 (8.5%, 95% CI 7.0%-10.3%) had confirmed cases. Of these, 94 were working in an 11th-floor call center with 216 employees, translating to an attack rate of 43.5% (95% CI 36.9%-50.4%). The household secondary attack rate among symptomatic case-patients was 16.2% (95% CI 11.6%- 22.0%). Of the 97 persons with confirmed COVID-19, only 4 (1.9%) remained asymptomatic within 14 days of quarantine, and none of their household contacts acquired secondary infections. Extensive contact tracing, testing all contacts, and early quarantine blocked further transmission and might be effective for containing rapid outbreaks in crowded work settings.
[23] Cheng H, Jian S, Liu D, et al. Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan and Risk at Different Exposure Periods Before and After Symptom Onset. JAMA Intern Med. 2020;180(9):1156-1163. doi:10.1001/jamainternmed.2020.2020: https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2765641 : In this case-ascertained study of 100 cases of confirmed COVID-19 and 2761 close contacts, the overall secondary clinical attack rate was 0.7%. The attack rate was higher among contacts whose exposure to the index case started within 5 days of symptom onset than those who were exposed later. Among the 91 close contacts of the 9 asymptomatic cases, no secondary transmission was observed.
[24] COVID-19 transmission–up in the air The Lancet Respiratory Medicine Crossref DOI link: https://doi.org/10.1016/S2213-2600(20)30514-2 Published: 2020-12 : Respiratory viruses are transmitted in three main ways. First, contact transmission, where someone comes into direct contact with an infected person or touches a surface that has been contaminated. Second, through droplet transmission of both large and small respiratory droplets that contain the virus, which would occur when near an infected person. Third, through airborne transmission of smaller droplets and particles that are suspended in the air over longer distances and time than droplet transmission. Initially it was thought that airborne transmission of SARS-CoV-2 was unlikely, but growing evidence has highlighted that infective microdroplets are small enough to remain suspended in the air and expose individuals at distances beyond 2 m from an infected person. This knowledge is also corroborated by investigation of spread of cases between people who were not in direct or indirect contact, suggesting that airborne transmission was the most likely route. In July, over 200 scientists published a statement calling for international bodies to recognise the potential for airborne spread of COVID-19 as they were concerned that people would not be fully protected by adhering to the current recommendations.
[25] Outdoor Transmission of SARS-CoV-2 and Other Respiratory Viruses: A Systematic Review J Infect Dis. 2021 Feb 24;223(4):550-561. doi: 10.1093/infdis/jiaa742: Five identified studies found a low proportion of reported global SARS-CoV-2 infections occurred outdoors (<10%) and the odds of indoor transmission was very high compared to outdoors (18.7 times; 95% confidence interval, 6.0-57.9). Existing evidence supports the wide-held belief that risk of SARS-CoV-2 transmission is lower outdoors but there are significant gaps in our understanding of specific pathways.
[26] https://www.lci.fr/sante/video-covid-19-le-port-du-masque-a-l-exterieur-est-il-utile-2162627.html: Risque de contagion très faible en extérieurs.
[27] Association between living with children and outcomes from covid-19: OpenSAFELY cohort study of 12 million adults in England, BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n628 (Published 18 March 2021): Among 9 334 392adults aged 65 years and under, during wave 1, living with children was not associated with materially increased risks of recorded SARS-CoV-2 infection, covid-19 related hospital or intensive care admission, or death from covid-19. In wave 2, among adults aged 65 years and under living with children was associated with a very small increased risk, e.g., in the number of hospital admissions of 1-5 per 10 000 people from 160 to between 161 and 165 (children aged 0-11) and with an increase of an increase of 2-6 per 10 000 (children aged 12-18 years).
[28] Kao T.W., Huang K.C., Huang Y.L., Tsai T.J., Hsieh B.S., Wu M.S. The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease. J Formos Med Assoc. 2004;103:624-628. https://pubmed.ncbi.nlm.nih.gov/15340662/ : Thirty nine patients (23 men; mean age, 57.2 years) were recruited for participation in the study. Seventy percent of the patients showed a reduction in partial pressure of oxygen (PaO2), and 19% developed various degrees of hypoxemia. Wearing an N95 mask significantly reduced the PaO2 level (101.7 +/- 12.6 to 92.7 +/- 15.8 mm Hg, p = 0.006), increased the respiratory rate (16.8 +/- 2.8 to 18.8 +/- 2.7/min, p < 0.001), and increased the occurrence of chest discomfort (3 to 11 patients, p = 0.014) and respiratory distress (1 to 17 patients, p < 0.001). Baseline PaO2 level was the only significant predictor of the magnitude of PaO2 reduction (p < 0.001). Conclusion: Wearing an N95 mask for 4 hours during HD significantly reduced PaO2 and increased respiratory adverse effects in ESRD patients.
[29] Beder A., Buyukkocak U., Sabuncuoglu H., Keskil Z.A., Keskil S. Preliminary report on surgical mask induced deoxygenation during major surgery. Neurocirugia (Astur) 2008;19:121-126. https://pubmed.ncbi.nlm.nih.gov/18500410/ :This study was undertaken to evaluate whether the surgeons’ oxygen saturation of hemoglobin was affected by the surgical mask or not during major operations. Repeated measures, longitudinal and prospective observational study was performed on 53 surgeons using a pulse oximeter pre and postoperatively. Our study revealed a decrease in the oxygen saturation of arterial pulsations (SpO2) and a slight increase in pulse rates compared to preoperative values in all surgeon groups. The decrease was more prominent in the surgeons aged over 35.
[30] Ong J.J.Y., Bharatendu C., Goh Y., Tang J.Z.Y., Sooi K.W.X., Tan Y.L. Headaches Associated With Personal Protective Equipment – A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache. 2020;60:864-877. [PubMed] [Google Scholar] : Coronavirus disease 2019 (COVID-19) is an emerging infectious disease of pandemic proportions. Healthcare workers in Singapore working in high-risk areas were mandated to wear personal protective equipment (PPE) such as N95 face mask and protective eyewear while attending to patients. Most healthcare workers develop de novo PPE-associated headaches or exacerbation of their pre-existing headache disorders.
[32] Kieran Dee, Daniel M Goldfarb, Joanne Haney, Julien A R Amat, Vanessa Herder, Meredith Stewart, Agnieszka M Szemiel, Marc Baguelin, Pablo R Murcia, Human rhinovirus infection blocks SARS-CoV-2 replication within the respiratory epithelium: implications for COVID-19 epidemiology, The Journal of Infectious Diseases, 2021;, jiab147, https://doi.org/10.1093/infdis/jiab147: Virus-virus interactions influence the epidemiology of respiratory infections.
However, the impact of viruses causing upper respiratory infections on SARS-CoV-2 replication and transmission is currently unknown. Human rhinoviruses cause the common cold and are the most prevalent respiratory viruses of humans. Interactions between rhinoviruses and co-circulating respiratory viruses have been shown to shape virus epidemiology at the individual host and population level. Here, we examined the replication kinetics of SARS-CoV-2 in the human respiratory epithelium in the presence or absence of rhinovirus. We show that human rhinovirus triggers an interferon response that blocks SARS-CoV-2 replication. Mathematical simulations show that this virus-virus interaction is likely to have a population-wide effect as an increasing prevalence of rhinovirus will reduce the number of new COVID-19 cases.
[33] Review report Corman-Drosten et al. Eurosurveillance 2020, November 27, 2020, https://cormandrostenreview.com/report/ : There are ten fatal problems with the Corman-Drosten paper which we will outline and explain in greater detail in the following sections: Problem 3. The number of amplification cycles (less than 35; preferably 25-30 cycles); In case of virus detection, >35 cycles only detects signals which do not correlate with infectious virus as determined by isolation in cell culture [reviewed in 2]; if someone is tested by PCR as positive when a threshold of 35 cycles or higher is used (as is the case in most laboratories in Europe & the US), the probability that said person is actually infected is less than 3%, the probability that said result is a false positive is 97%.
[34] WHO Information Notice for IVD Users 2020/05. Nucleic acid testing (NAT) technologies that use polymerase chain reaction (PCR) for detection of SARS-CoV-2. Date: 13 January 2021. https://www.who.int/news/item/20-01-2021-who-information-notice-for-ivd-users-2020-05 : WHO guidance Diagnostic testing for SARS-CoV-2 states that careful interpretation of weak positive results is needed (1). The cycle threshold (Ct) needed to detect virus is inversely proportional to the patient’s viral load. Where test results do not correspond with the clinical presentation, a new specimen should be taken and retested using the same or different NAT technology. WHO reminds IVD users that disease prevalence alters the predictive value of test results; as disease prevalence decreases, the risk of false positive increases (2). This means that the probability that a person who has a positive result (SARS-CoV-2 detected) is truly infected with SARS-CoV-2 decreases as prevalence decreases, irrespective of the claimed specificity. Most PCR assays are indicated as an aid for diagnosis, therefore, health care providers must consider any result in combination with timing of sampling, specimen type, assay specifics, clinical observations, patient history, confirmed status of any contacts, and epidemiological information.
[35] Clarifying the evidence on SARS-CoV-2 antigen rapid tests in public health responses to COVID-19, February 17, 2021DOI:https://doi.org/10.1016/S0140-6736(21)00425-6, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)00425-6/fulltext : Testing for SARS-CoV-2 is central to COVID-19 management and has relied on quantitative reverse transcriptase polymerase chain reaction (PCR) technology. PCR seeks the genetic code of the virus from nose or throat swabs and amplifies it over 30-40 cycles, doubling each cycle, enabling even miniscule, potentially single, copies to be detected. PCR is thus a powerful clinical test, specifically when a patient is, or was recently, infected with SARS-CoV-2. Fragments of RNA can linger for weeks after infectious virus has been cleared,6 often in people without symptoms or known exposures. Most people infected with SARS-CoV-2 are contagious for 4-8 days.7 Specimens are generally not found to contain culture-positive (potentially contagious) virus beyond day 9 after the onset of symptoms, with most transmission occurring before day 5.7, 8 This timing fits with the observed patterns of virus transmission (usually 2 days before to 5 days after symptom onset), which led public health agencies to recommend a 10-day isolation period.9 The short window of transmissibility contrasts with a median 22-33 days of PCR positivity (longer with severe infections and somewhat shorter among asymptomatic individuals).10 This suggests that 50-75% of the time an individual is PCR positive, they are likely to be post-infectious.11, 12 Once SARS-CoV-2 replication has been controlled by the immune system, RNA levels detectable by PCR on respiratory secretions fall to very low levels when individuals are much less likely to infect others.13, 14, 15 The remaining RNA copies can take weeks, or occasionally months,16, 17 to clear, during which time PCR remains positive.
[36] Sensational judgment in Austria: PCR test not suitable as proof of infection. https://reitschuster.de/post/sensations-urteil-in-oesterreich-pcr-test-nicht-zum-infektions-nachweis-geeignet/
[37] J. P A Ioannidis, Infection fatality rate of COVID-19 inferred from seroprevalence data https://www.who.int/bulletin/volumes/99/1/20-265892/en/: Findings: I included 61 studies (74 estimates) and eight preliminary national estimates. Seroprevalence estimates ranged from 0.02% to 53.40%. Infection fatality rates ranged from 0.00% to 1.63%, corrected values from 0.00% to 1.54%. Across 51 locations, the median COVID-19 infection fatality rate was 0.27% (corrected 0.23%): the rate was 0.09% in locations with COVID-19 population mortality rates less than the global average (500 COVID-19 deaths/million people. In people younger than 70 years, infection fatality rates ranged from 0.00% to 0.31% with crude and corrected medians of 0.05%. Conclusion: The infection fatality rate of COVID-19 can vary substantially across different locations and this may reflect differences in population age structure and case-mix of infected and deceased patients and other factors. The inferred infection fatality rates tended to be much lower than estimates made earlier in the pandemic.
[38] Fauci A.S., Lane H.C., Redfield R.R. Covid-19 – Navigating the Uncharted. N Engl J Med. 2020;382:1268-1269. https://www.nejm.org/doi/full/10.1056/nejme2002387: If one assumes that the number of asymptomatic or minimally symptomatic cases is several times as high as the number of reported cases, the case fatality rate may be considerably less than 1%. This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.
[39] Covid-19 laissons les médecins prescrire : https://stopcovid19.today/
[40] « Un plan simple pour éradiquer le nouveau coronavirus de Belgique » (Marc Wathelet) : https://www.lespecialiste.be/fr/debats/ldquo-un-plan-simple-pour-eradiquer-le-nouveau-coronavirus-de-belgique-rdquo-marc-wathelet.html?